I'm back again with a dorky song. Written originally years ago for undergraduate Microbiology Lab, this song was in response to the many outbreaks of E. coli (specifically those occuring in spinach and other produce).
I hope you find this song as enjoyable as I do.
I would love to hear some feedback on this and the other "performances" I have posted under the "Phage Fun" heading. Feel free to e-mail me at the address on the left.
It's Gonna Be There (The E. Coli Song) To the tune of Blessid Union of Souls' "I Wanna Be There"
Lyrics
Don't you let that burger fall
I really hope you washed your hands
Invisible to eyes, that means small
Is that too hard to understand.
You got to clean everything
Or it will be filled with coliforms
And pretty soon, someone may be dead.
Chorus
It's gonna be there when you zip your fly
It's gonna be there when you rub your eyes
It'll cramp your stomach, cause internal pain
It'll make your intestines go insane.
It's gonna be on beef, whether or steak or ground
And in leafy greens it has been found
You better cook your food
You better wash your hands
Cause E. coli's on the lamb
You'd never know that it was there
But it has been there all the time
And if it had its way, it stay in cows on farms
But it loves bad hygeine and your grime
Cause you got dirt on yourself
When you leave the toilet room
Though the sign says, "Employees Wash Your Hands"
Chorus
And if its got blood cells to kill
Well you'd have to take some pills
And with some time, your kidneys may fail
It's gonna be there when you zip your fly
It's gonna be there you don't have to try
Gram negative and anaerobic too
And it lives inside of me and you
It's gonna be there on your burger
It's gonna be there on your knife
It'll cramp your stomach, cause internal pain
It'll make your intestines go insane.
Other Songs to Listen To:
The Brillant Dance of the Starvation Response
The Ballad of the Virus (They're Everywhere)
I've Got You Phage
Thursday, October 23, 2008
Friday, October 17, 2008
The Origins of Antibiotic Resistance
One way to do this is to look for functional antibiotic resistance genes in a bacterial population that has not been exposed to our medical treatment pressures. Researchers from the University of Wisconsin-Madison recently published an article that shows just this. They have demonstrated that antibiotic resistance genes (specifically those which encode beta-lactamases) can be found in soil bacteria from pristine regions of Alaska.

Using soil cores from a region of Bonanza Creek Experimental Forest, the researchers extracted bacterial DNA. This was then cloned into a library and constructs were screened for resistance to beta-lactamase. Those constructs that were positive for resistance were then subjected to transposon mutagenesis to identify the precise region conferring resistance.
Not only does this demonstrate that beta-lactamases were present, but more importantly, it demonstrated that these genes were functional. This is a far leap up from merely metagenomic sequencing. A sequence may be able to tell you if a type of gene is present, but it can not tell you if it is functional. Furthermore, merely sequencing may hide the presence of a beta-lactamase that has no homology to known genes.
Of the nearly 12 Gigabases of DNA that they extracted, they isolated 14 clones that had the ability to grow on clinically significant concentrations of beta-lactam antibiotics. The genes encoded by these clones were found to be distantly related to the current bank of known beta-lactamases. This allows us to have a look back in time to see the functional beta-lactamases that gave rise to the types in our current strains.
(The authors also found the first example of a bifunctional beta-lactamase. That is, a single protein created by the fusion of two different, yet functional, beta-lactamases. Perhaps an example of duplication giving rise to a new subset?)
I am a firm believer in the fact that in order to know where we are going, we must always remember where we came from. On that note, in order to provide better answers to antibiotic resistance, we must first understand how it arose.
Allen, H., Moe, L., Rodbumrer, J., Gaarder, A., & Handelsman, J. (2008). Functional metagenomics reveals diverse β-lactamases in a remote Alaskan soil The ISME Journal, 3 (2), 243-251 DOI: 10.1038/ismej.2008.86
Other articles of interest:
Altruism in Bacteria? Allowing Yourself to Die for the Good of the Species
Wild Bacteria That Eat Our Antibiotics?! Of Course!
Sunday, October 5, 2008
A MAP to Crohn's Disease; Revisiting Koch's Postulates
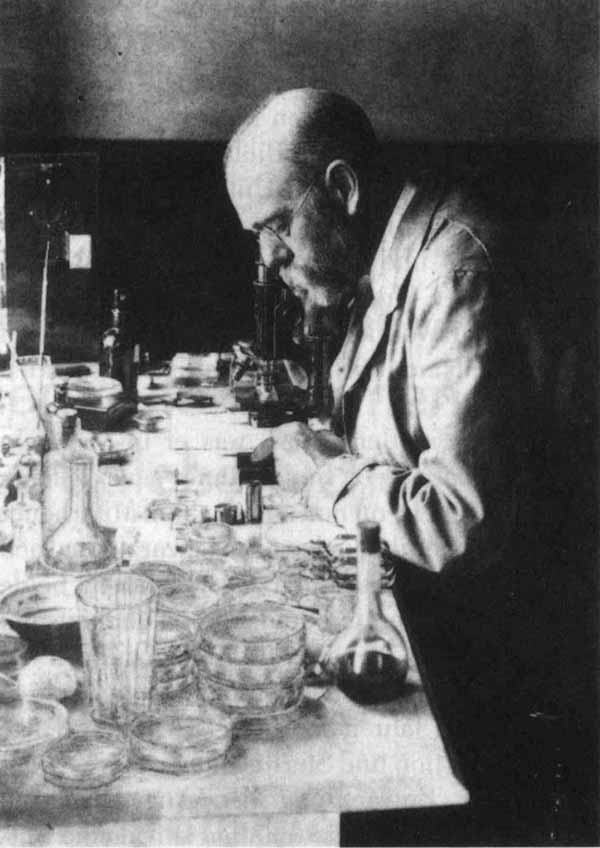 The fundamental principle of infectious disease is Koch'sPostulate. To be brief, he set forth the qualifications that must be fulfilled in order to associate a pathogen with an illness. This includes the isolation of the organism from diseased tissue, the ability to grow the organism in pure culture, and the recreation of the disease in a healthy individual following introduction of the purified organism.
The fundamental principle of infectious disease is Koch'sPostulate. To be brief, he set forth the qualifications that must be fulfilled in order to associate a pathogen with an illness. This includes the isolation of the organism from diseased tissue, the ability to grow the organism in pure culture, and the recreation of the disease in a healthy individual following introduction of the purified organism.This procedure was used at the time to demonstrate Mycobacterium tuberculosis as the causative agent of consumption. Although to be sure, Koch's Postulate does run into some trouble with organisms such as M. leprae which can not be grown ex vivo. (More on M. leprae's reductive genome found here)
It is only fitting that a modern day example of pathogen associated disease is that of another mycobacteria, the intracellular pathogen M. avium paratuberculosis (MAP) and its potential to be a causative agent of Crohn's Disease.
Crohn's Disease is a severe inflammatory bowel syndrome, characterized by inflammation in discrete sections of intenstinal tissue seperated by healthy tissue. Affecting over half a million people in our country (CDC 2001), this chronic illness has no known cure. Treatments include anti-inflammatory drugs, and tellingly, the anti-mycobacterial rifampicin.
A recent study from the University of Otago in New Zealand has shown a strong correlation between the presence of MAP and Crohn's Disease. Using a PCR detection method, they amplified a region specific to MAP, the IS900 element, from white bloodcells of both Crohn's patients and non-affected individuals. The PCR screen is sensitive enough to detect 100 cells/mL of blood. Furthermore, this study is currently the largest of it's kind, examining samples from over 350 affected individuals and 200 controls. Past studies have only looked at groups of around 50 individuals.

Owing to the larger number of samples, this study lends itself to a more detailed statistical analysis. Firstly they found that 122 of the 361 individuals (33.8%) affected by Crohn's were postive for MAP. On the otherhand, 43 of the 200 control samples (21.5%) were also MAP positive.
In my humble opinion, this does not seem significant. However, the author's statistical analysis shows otherwise. They show with a 95% confidence interval and a 0.002 p-value, that MAP is closely associated with Crohn's Disease. A handful of other (smaller) studies have confirmed similar results. However, the conclusion remains controversial due to many other studies that have not found a correlation.
A close friend has said that this study reminds him of the Heliobacter pylori and stomach ulcer story (of Nobel Prize winning proportions). However, a fundamental difference between that story and this one, is that we have yet to show that a pure culture of MAP is capable of inducing pathology in an individual. (Although it is the causative agent of a bovine inflammatory bowel syndrome)
***Revision 17 Oct 2008: An astute reader pointed out that Dr. Rod Chiodini has already fulfilled Koch's Postulates for MAP-induced Crohn's Disease. A little digging found the article: Dig Dis Sci. 1986 Dec;31(12):1351-60. MAP from Crohn's patients was isolated and used to induce the bowel disease in goats! ***
It is my belief that we will find that MAP is not the sole agent of Crohn's, but is likely an instigator for many individuals who are genetically pre-disposed to inflammatory disease. We are peeling back more knowledge each day that demonstrates that disease isn't as simple as an invading pathogen. Stochasticity and host response must be taken into account when determining the cause of disease.
Source:
Bentley, R., Keenan, J., Gearry, R., Kennedy, M., Barclay, M., & Roberts, R. (2008). Incidence of Mycobacterium avium Subspecies paratuberculosis in a Population-Based Cohort of Patients With Crohn's Disease and Control Subjects The American Journal of Gastroenterology, 103 (5), 1168-1172 DOI: 10.1111/j.1572-0241.2007.01742.x
Other articles of interest:
Reductive Evolution in Mycobacterium leprae
A Brief Bit More on Reductive Evolution in M. leprae
Subscribe to:
Posts (Atom)


